Welcome to a sweet journey of discovery, folks! Today, we will explore the mysterious world of diabetes, where sugar, insulin, and healthy living intertwine in a fascinating dance. So grab your glucometers, slip into your comfiest sneakers, and let’s take a deep dive into understanding the ins and outs of diabetes. Enjoy our first of many collaborations with Angela Debartolome, MS in Nutrition and Dietetics, Dietetic Intern. Ms. Debartolome has given us insight and knowledge to pass along to our readers to give a better understanding.
Chapter 1: What is Diabetes?
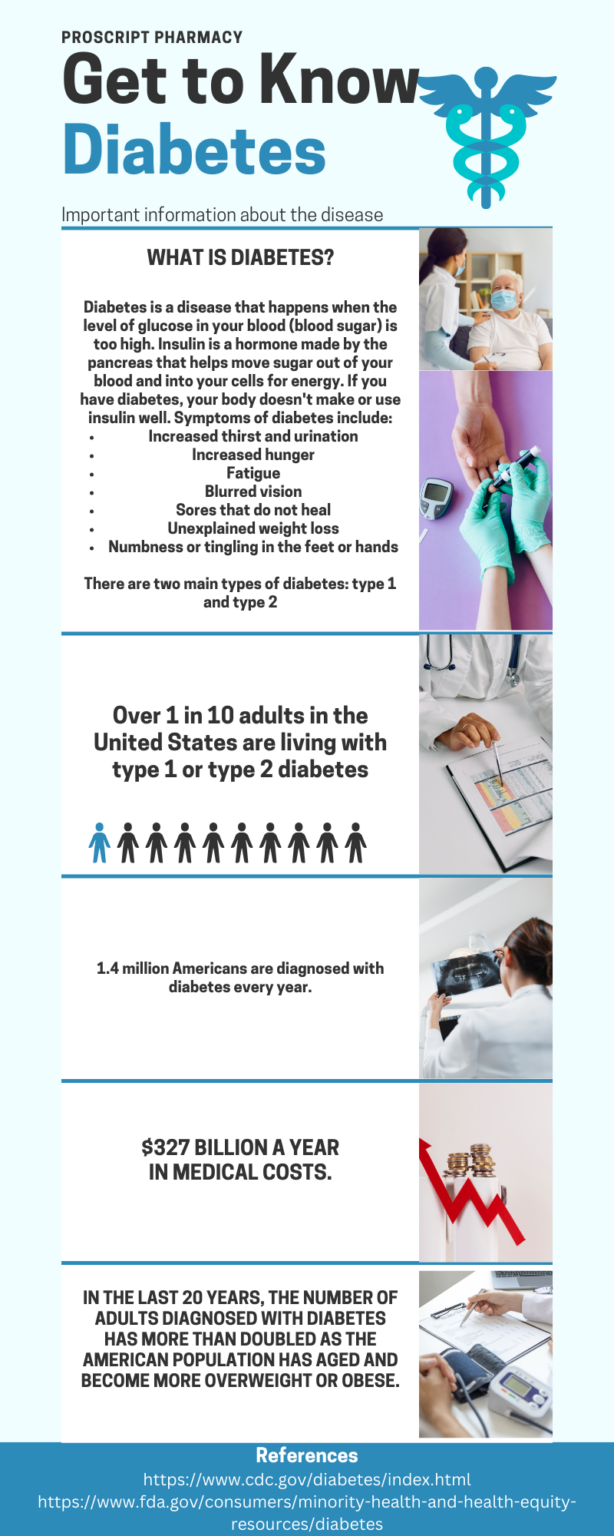
We can’t dive into the deep end without first understanding what diabetes is. Think of it as a body’s complicated relationship with what you’ll hear termed as glucose but is also referred to as sugar. In simple terms, it’s a condition that affects how your body manages blood sugar levels. There are two main types: Type 1, where your body doesn’t produce enough insulin, and Type 2, where your body doesn’t use insulin effectively. It’s like your body’s sugar thermostat is acting a little wonky.
Type 1 diabetes occurs when the pancreas can’t produce insulin or produces very little insulin because specific vital cells within the pancreas are harmed, usually stemming from a genetic element.When cells can’t take in glucose, two things can occur: the sugar levels in the blood go up, and the cells don’t get the food they need. This leads to the liver making more glucose, which further increases the sugar levels in the blood. In response to this, you might experience symptoms of increased thirst or frequent urination, which, along with bloodwork, are the two most common indications of T1DM.
While Type 1 diabetes happens because the body doesn’t make insulin, Type 2 diabetes is different.
In Type 2 diabetes, the body does make insulin. Still, the problem is that the body’s cells don’t respond to it appropriately. This means the body needs more insulin, and the pancreas works harder. Over time, the pancreas can’t keep up. This makes it hard for the body to use insulin. When the cells can’t use insulin, they can’t take in glucose from the blood for energy. Obesity, poor nutrition, and physical inactivity are the three primary factors that play a role in the development of T2DM.
Chapter 2: The Sugar Chronicles
Now, let’s get to the nitty-gritty of it all – sugar! We all love it, but for folks with diabetes, managing it is crucial. Sugar isn’t the enemy, but balance is the key. Learn about the importance of carbohydrates, the role of glucose, and how they all fit into this sugary puzzle. Carbs play a crucial role in diabetes management because they have a significant impact on blood sugar levels. When glucose is released into the bloodstream, it raises blood sugar levels. In a person without diabetes, the pancreas automatically releases insulin, a hormone, in response to the rising blood sugar levels. Insulin helps glucose, used for energy, enter the body’s cells.
Chapter 3: The Insulin Hero
Meet the unsung hero of our tale, insulin. Insulin is the key that unlocks the door for sugar to enter your cells, providing them with the energy they need. In diabetes, this hero faces some challenges. For Type 1, it’s in short supply, and for Type 2, the key isn’t turning as smoothly as it should. Please speak to your doctor to see how medication, diet, and lifestyle changes can help insulin do its job. People with Type 1 diabetes need to rely on daily insulin injections, along with a balanced diet and exercise, to replicate the natural insulin production in someone without diabetes. Effective insulin management involves regularly checking glucose levels and making necessary changes to insulin doses, food choices, and physical activity.
In the case of Type 2 diabetes, as it advances, medications that lower blood sugar become necessary if maintaining good glucose control through lifestyle measures, such as nutrition and exercise, is no longer possible.
Chapter 4: Monitoring Magic
Diabetes management is like being a detective, continuously monitoring your blood sugar levels. A glucometer is a portable device used to measure the concentration of glucose (sugar) in a person’s blood. It works by collecting a small blood sample and analyzing it on a disposable test strip inserted into the meter. Within seconds, the meter displays the blood glucose level. It is a great way to track it. It’s like having your sugar scoreboard.
Chapter 5: Dining with Diabetes
Eating with diabetes doesn’t mean giving up on deliciousness. Discover the approaches to managing your diabetes and explore recipes designed for people with diabetes. People with diabetes often use carbohydrate (carb) counting as a key strategy to manage their blood sugar. Carb counting is based on the idea that the carbohydrates in our food have the most significant impact on our blood sugar levels. The key is to aim for consistent carbohydrate amounts in your meals and snacks, making it a straightforward method for meal planning. Carbs come from various sources like starches, fruits, milk and yogurt, and sweet treats. You can count carbs in one of these three ways:
1. Each serving of food with 15 grams of carbohydrates is considered one carbohydrate choice.
2. You can calculate the total grams of carbohydrates in a meal or snack using the information provided on food labels.
3. There are online and mobile applications available to help you monitor your carbs intake, and many of them can even connect with insulin pumps and self-monitoring blood glucose (SMBG) devices for added convenience.
By tracking the amount of carbs you consume, practitioners can better match your insulin or medication dosage to the carbohydrate intake, helping maintain stable blood sugar levels. A glycemic index measures how quickly carbohydrates in food raise blood sugar levels. Foods with a high glycemic index cause a rapid increase in blood sugar, while low-glycemic index foods have a more gradual effect. People with diabetes can use the glycemic index to choose carbohydrates that have a milder impact on blood sugar.
What’s the most popular and helpful advice I give to my patients? Consume high-fiber foods. Fiber is a type of carbohydrate that has a minimal impact on blood sugar. High-fiber foods can help regulate blood sugar levels, improve insulin sensitivity, and promote a feeling of fullness, aiding in weight management. Some high-fiber foods are whole grains, legumes, fruits like apples and pears, vegetables like broccoli and spinach, and nuts and seeds. A quick meal example would be a warm oatmeal prepared with almond milk sweetened with granny smith apples – great for the fall weather, too!
Below, you will see three links: One will bring you to a “cheat sheet” provided by the American Diabetes Association that shares all things related to carbohydrate counting and diabetes. The second will bring you to a website that will teach you how to read food labels properly. Lastly, the third link will provide you with easy-to-make meals to help you control your diabetes!
https://diabetes.org/food-nutrition/understanding-carbs/carb-counting-and-diabetes
https://www.everydayhealth.com/type-2-diabetes/diet/delicious-diabetes-friendly-dinner-ideas/
Chapter 6: Exercise and Diet: A Power Couple
Exercise and proper diet when aiding in the treatment of diabetes are like Batman and Robin – a dynamic duo. Both parameters help to regulate blood sugar levels, improve insulin sensitivity, and support weight management. Moreover, regular exercise improves cardiovascular health, enhances insulin sensitivity, and reduces stress levels. Both aerobic and strength training exercises can be beneficial for diabetes management. It is recommended that:
• Children with diabetes should be encouraged to engage in at least 60 minutes of physical activity each day
• Adults with diabetes should be advised to perform at least 150 minutes/week of moderate-intensity aerobic activity, spread over at least 3 days/week with no more than 2 consecutive days without exercise
• Adults with T2DM should be encouraged to perform resistance training at least twice per week
Remember that both low and high blood sugar are acute risks of exercise. Blood glucose levels should be monitored, carbohydrates should be increased, and/or insulin adjustments should be made if applicable. For moderate exercise lasting less than 30 minutes, additional carbohydrate or insulin adjustment is rarely necessary. On the other hand, if blood glucose levels are within normal limits and expertise will last longer than 30 minutes, a small snack may be needed. As a general rule of thumb, an additional 15 g of carbohydrates should be adequate for 1 hour of moderate physical activity. For more strenuous exercise, 30 g of carbohydrates per hour may be required.
A diabetic diet is a crucial part of managing both Type 1 Diabetes (T1DM) and Type 2 Diabetes (T2DM). While the basic principles of a diabetic diet are similar for both types, there may be variations based on individual needs and treatment plans. Here are some general dietary guidelines for T1DM and T2DM:
1. Carbohydrate Management:
• Monitor carbohydrate intake, as carbohydrates have the most direct impact on blood sugar levels.
• Focus on complex carbohydrates like whole grains, vegetables, and legumes, which have a lower glycemic index and result in slower blood sugar increases.
• Be consistent with carbohydrate intake throughout the day to help stabilize blood sugar levels.
2. Portion Control:
• Pay attention to portion sizes to avoid overeating, which can lead to blood sugar spikes.
• Use measuring cups or a food scale if needed to ensure accurate portion control.
3. Fiber-Rich Foods:
• Include high-fiber foods like whole grains, vegetables, fruits, and legumes.
• Fiber helps regulate blood sugar levels and promotes a feeling of fullness.
4. Lean Protein:
• Incorporate lean protein sources like poultry, fish, tofu, and legumes into your meals.
• Protein can help stabilize blood sugar and keep you feeling satisfied.
5. Healthy Fats:
• Choose unsaturated fats like olive oil, avocados, and nuts while limiting saturated and trans fats.
• Healthy fats are essential for heart health and overall well-being.
6. Sugar and Sweeteners:
• Limit added sugars and sugary foods.
• Use sugar substitutes in moderation if recommended by your healthcare provider.
Chapter 7: Diabetes Superheroes
Diabetes affects people from all walks of life. You’re not the only one dealing with this condition, as it is the most prevalent among all endocrine disorders. More than 30 million individuals have already received a diabetes diagnosis, and this number is steadily increasing. From athletes to actors, they’ve shown that diabetes doesn’t have to limit your dreams. Their stories will inspire and uplift you.
Chapter 8: Wrapping it All Up
As we come to the end of our journey, remember that diabetes is an opportunity to take charge of your health, embrace a healthier lifestyle, and learn to live life to the fullest. With knowledge and support, you can turn your diabetes journey into an incredible adventure.
Remember to speak to your doctors and dietitians to dive deeper into diabetes. These practitioners work hand in hand to come up with the best course of treatment for your individualized journey with diabetes.